HIPAA Compliance is critical for organizations in the healthcare sector, ensuring that the privacy and security of patient data are maintained according to strict federal standards. The Health Insurance Portability and Accountability Act (HIPAA) mandates that healthcare providers, insurers, and their business associates take the necessary steps to safeguard Protected Health Information (PHI). Failing to comply with HIPAA can result in severe financial penalties and reputational damage.
One of the most significant risks of non-compliance with HIPAA is the financial penalties imposed by the U.S. Department of Health and Human Services (HHS). The fines for failing to meet HIPAA standards can be substantial and vary depending on the severity of the violation.
Tier 1 violations, which are due to a lack of knowledge or understanding, can incur fines up to $50,000 per violation, with a maximum penalty of $1.5 million per year. More serious violations, such as willful neglect of HIPAA rules, can result in fines reaching $100,000 per violation, with a total annual penalty of up to $1.5 million.
The potential for these hefty fines underscores the importance of adhering to HIPAA standards. Beyond financial penalties, non-compliance can lead to damaged reputations, loss of patient trust, and lawsuits. The checklist helps businesses understand the key components of HIPAA compliance, from conducting risk assessments to implementing proper data encryption, ultimately supporting efforts to avoid fines and maintain a secure environment for sensitive health information.
This comprehensive guide is written for businesses looking to ensure they meet the stringent requirements of HIPAA. This resource provides a step-by-step framework to help organizations navigate the complexities of HIPAA compliance, including the administrative, technical, and physical safeguards needed to guard protected health information (PHI). By following this checklist, healthcare organizations can take the necessary actions to avoid costly mistakes and ensure they stay within legal boundaries.
What is HIPAA?
HIPAA was put in place to regulate the handling of protected health information. The act created industry-wide standards for data handling, cybersecurity, insider, access, and electronic billing. One of the most important regulations to emerge from the rules was that medical data must remain confidential.
The regulations apply to covered entities, insurance providers, and clearinghouses (that process transactions between covered entities and insurance providers). If the care provider doesn’t submit an electronic transaction for insurance payment for the treatment provided to patients then HIPAA doesn’t apply to them.
It is also worth noting the role of business associates. Business associates are companies that provide services that require persistent access to protected health information and are subject to the regulations.
The idea behind HIPAA is that patient data should be protected from fraudsters and other malicious entities. In the age of cloud computing; the range of entry points makes protecting this data a complex issue. All of your physical and virtual resources need to be secured against cyber attackers to protect patient data.
However, becoming HIPAA compliant is not just a question of network security, but of internal access as well. You must have plans in place to control internal access to patient data and ensure staff adheres to minimum use and disclosure requirements.
These restrictions were put in place to enable the Healthcare industry to reduce the improper disclosure of patient information. All staff and business associates must make sure to work alongside your network security processes, and not rely on them alone to protect patient data.
The HIPAA Privacy Rule
The HIPAA Privacy Rule dictates how PHI can be accessed and handled. The rule only applies to covered entities and states that there must be procedures in place to protect the privacy of patient data. However, privacy rule requirements can also be incorporated into business associate agreements.
Beyond the basic requirement to protect patient data, enterprises also have to support the rights that patients have to that data. There are three rights outlined in HIPAA that all patients have the right to:
- authorize disclosure of their PHI
- request access to a copy of their health records at any time
- request corrections to their records
To break it down further, the HIPAA Privacy Rule states that consent is required from the patient in order to disclose PHI data. In the event that a patient requests access to their data, organizations have 30 days to respond. Failing to respond on time can leave an enterprise open to legal liabilities and potential fines.
The HIPAA Security Rule
The HIPAA Security Rule is a security requirement that outlines how ePHI should be managed. The rule stipulates that enterprises should “implement the necessary safeguards” to protect patient data. The HIPAA Security Rule and the HIPAA Privacy Rule are closely related but separate, as they were implemented three years apart.
While the safeguards themselves are not ambiguous, how an entity determines the level of “necessary safeguards” and addresses those in a reasonable and appropriate manner is more complex. To help simplify the requirements, HIPAA breaks down the safeguards into three main sections:
- Administrative safeguards
- Technical safeguards
- Physical safeguards
Administrative Safeguards
The HIPAA Security Rule defines administrative safeguards as “administrative actions, and policies and procedures to manage the selection, development, implementation, and maintenance of security measures to protect electronic health information.” It also states that managing the conduct of the workforce comes as part of that responsibility.
Administrative safeguards suggest that enterprises must implement administrative processes that control access to patient data and provide additional training to enable employees to interact with information securely. To manage workforce conduct an employee should be appointed to manage HIPAA policies and procedures.
Physical Safeguards
The physical safeguards requirement is about securing the facilities where patient data is located and the resources used to access the data. Controlling access to these areas is one of the major take-away messages of this section.
You need to have measures in place to control access to where patient data is processed, protect devices against unauthorized access (using methods such as two-factor authentication), and to control/record the movements of devices in or out of the facility.
Technical Safeguards
‘Technical safeguards’ is a term used to refer to the technical policies and procedures that protect patient data. Authentication, audit controls, audit reports, record keeping, access controls, and automatic logoffs are all measures that enterprises can implement to fulfill these criteria. There must also be measures in place to make sure that data is safe, whether it’s being stored in a device or being moved between locations.
The recent move of many commonly-used business tools to the cloud creates added complications over data protection for HIPAA compliance. The location of Microsoft 365, Google Workspaces, and other productivity suites that are frequently used to manage and access PHI mean that not only do your data stores need to be protected but the applications that access PHI regularly and the connections to them also need to be tightly protected. Fortunately, the emerging specialized hybrid system security field caters to these needs. You can get combined application access control and connection protection with systems such as Perimeter 81.
You should also complete a risk assessment to identify risk factors and threats to the security of ePHI data. You must then take measures to address these specific threats. The technical safeguards requirement is one of those areas where hiring a qualified HIPAA consultant will pay dividends as they will make sure there aren’t any gaps.
The Breach Notification Rule
The Breach Notification Rule specifies how enterprises should respond to data breaches. The rule states that organizations must notify individuals, the media or the HHS Secretary in the event of a data breach. A breach is defined as “an impermissible use or disclosure under the Privacy Rule that compromises the security or privacy of the protected health information”.
Following a breach, you should notify the necessary parties ASAP but no later than 60 days after the event. When writing up the notification you will need to state: what personal identifiers were exposed, the individual who used the ePHI, whether the ePHI was acquired or viewed, and whether the risk of damage has been mitigated.
Reporting is another integral component of The Breach Notification Rule. Smaller breaches affecting less than 500 individuals need to be reported through the HHS website annually (if more than 500 individuals are affected you need to contact the media as well). Monitoring breaches closely on a case-by-case basis to assess the damage and respond accordingly is the key to success.
The Checklist
To help you stay compliant with HIPAA, we’ve compiled a brief list of steps you can take below. Please note that we recommend you enlist the assistance of an experienced HIPAA consultant to keep your data protected. Your consultant will be able to perform a full evaluation of your current security practices and identify areas to improve.
-
Complete a Risk Assessment
The first thing you need to do when preparing for HIPAA compliance is to assess the overall readiness of your enterprise. What you need to do to comply with the regulations depends on your current cybersecurity processes. Conducting a risk assessment that assesses how PHI and ePHI data is being managed will show you the gaps in your cybersecurity policy.
For the best results, work with a HIPAA compliance consultant. The consultant will assess your current practices against the requirements of the OCR Audit Protocol, and provide you with a list of recommendations to help achieve compliance. They will also tell you when you’re ready to start the certification process.
Working with an expert is beneficial because you will be able to rely on their experience to find vulnerabilities you may have overlooked. An experienced consultant will have a comprehensive grasp of HIPAA requirements and give you the best chance of achieving your certification.
-
Remediate Compliance Risks and Refine Processes
When the results of the initial assessment show that you have risk factors to address, it is time to change your processes. If you work with advisors to help you with the assessment, then they can provide you with specific guidance on the policies and procedures you need to implement.
To start with you will want to address smaller compliance issues before trying to follow through on larger targets. Implementing basic measures like training employees on cybersecurity practices, minimum use guidelines, disclosure guidelines, and how to use two-factor authentication on devices can help to start off on the right foot.
From there on you can start to set more complex remediation targets that will tell you which processes you need to prioritize. While network security is very important it is essential that employees are aware of the importance of internal access controls, and avoid disclosing patient information where possible.
-
Manage Risks Long Term (With Network Monitoring Tools)
Achieving HIPAA compliance isn’t a one-time effort but a consistent challenge. Your long term strategy will revolve around continually managing risks to make sure that patient data has been kept safe.
A network monitoring tool won’t get you compliant on it’s own, but it can help you to manage some of your risks (provided your internal access controls are adhered to by employees).
In particular, you want to use a tool that:
- uses vulnerability scans
- detects network events
- analyzes audit logs
- visualizes HIPAA components with a topology map
- monitors logons
- automates event analysis
- and automates compliance reporting.
While you can attempt to monitor HIPAA risks with multiple software products it is much easier to use a unified platform so you can manage everything in one place. Keep in mind that it only takes one vulnerability for an attacker to gain access to confidential data
Conditions of compliance
Problems arise when businesses outsource part of their data processing or data storage to external companies. Under these circumstances, the company is dependent on those managed service providers (MSPs) also being HIPAA compliant. Compliance, therefore, needs to be a condition in any contract signed for outsourced IT services.
The requirement of a chain of trust between a company under HIPAA obligations and the companies that serve it puts a great responsibility on MSPs. Without the ability to demonstrate HIPAA compliance, MSPs will not be able to bid for work from companies in the health sector. This creates san imperative for MSPs to become HIPAA compliant.
As discussed above, the easiest way to comply with HIPAA regulations is to buy in a platform of software products that already conform to HIPAA specifications.
MSPs need remote access utilities and system administration tools. They also require Help Desk platforms for both user access and technician support. The technician utilities in an MSP platform are collectively called a remote monitoring and management (RMM) system. The RMM tools have access to the entire client system and are responsible for backing up and archiving data and so they must be designed with HIPAA standards in mind.
The tools needed by the MSP to run its business include team management client management, and contract management. This category of utilities also requires a password vault to keep the access account details for each client – and keep them separate and secure. The MSP business management tools are known as “professional services automation” (PSA). As the PSA system includes access rights and sensitive information about client companies, this also needs to be compliant with HIPAA requirements.
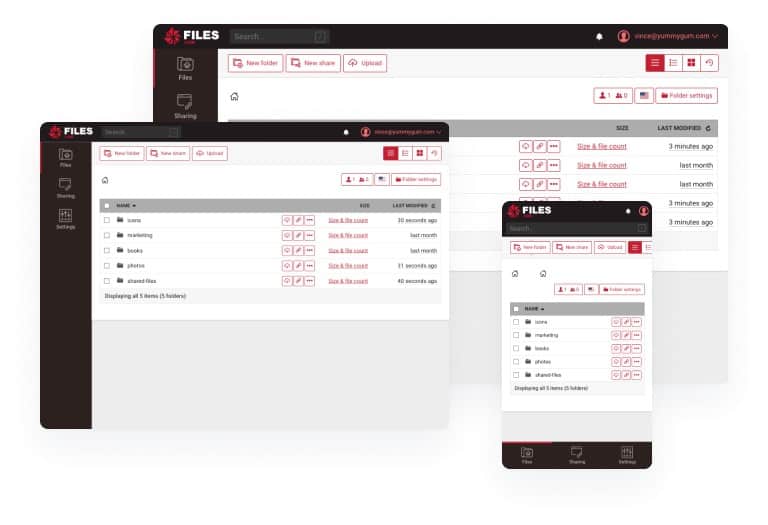
Files.com issues its customers with a BAA. The service operates as a file management system, including a file transfer and distribution service. While rival companies try to dodge HIPAA compliance, siting their role as a carrier, Files.com goes the full HIPAA compliance route.
You get a BAA with the service offered by ExaVault as well. This cloud storage platform is administered in data centers that implement sufficient physical security measures that earn the company ISO 27001 certification. You can get a 30-day free trial of ExaVault.
Consult an Experienced HIPAA Consultant
The challenges that come with complying with HIPAA are steep. A small oversight can result in the disclosure of private patient information. Reading up on the rules of the regulations and enlisting the help of an experienced HIPAA consultant will help you to implement the best protection for your enterprise and your patients.
Working with a consultant reduces the chance of any compliance gaps that could compromise PHI. While going alone is possible, there is a higher chance of misinterpreting the level of safeguards you need to protect patient data. An experienced consultant can make the process easier and close the door to financial liabilities.
HIPAA Compliance Checklist FAQS
What are the 5 steps toward HIPAA compliance?
Implement a HIPAA compliance plan in stages:
- Nominate a Privacy and Security Officer who will ensure that the plan is defined and implemented.
- Perform a risk assessment, which identifies system vulnerabilities, sensitive data locations and types, and third-party risk.
- Create privacy and security policies that specify system protection priorities
- Organize Business Associate Agreements that are a requirement from HIPAA to share responsibility with system suppliers that will handle data.
- Train employees in best practices and communicate the consequences of data disclosure.
What are the 10 most common HIPAA violations?
The 10 most common HIPAA violations are:
- Keeping unsecured records
- Not encrypting data.
- System intrusion
- Employee indiscretion
- Procedural misuse of data
- Employee misuse of data
- Data corruption or partial deletion that changes its meaning
- Inadequate activity tracking
- Cover-ups
- Insufficient protection of equipment that has access to data
What is the key to HIPAA compliance?
A common problem encountered when trying to achieve HIPAA compliance is that you can get let down by processes that are out of your control. This is third-party risk and it is concerned with the data security policies of the suppliers that you rely on. Examples of such third parties are cloud storage providers, data processing services, and managed service providers that monitor system performance. When your compliance is assessed, the performance of the companies you work with is included in the examination and this extends to the complies that support them if those lower tier services also process the sensitive data that you hold.
What information is protected by HIPAA?
HIPAA is concerned with the protection of health-related personal information of private individuals. This is known as “protected health information,” or PHI. While many data protection standards, such as GDPR, only extend to data held on digital media, HIPAA requires data security for all forms of data storage of usage, including paper records and also oral disclosure.